Feeding Tubes & Gastrostomies in Children
This resource discusses non-surgical and surgical feeding tubes, their differences, how they are placed, and common issues encountered in children with special health care needs. These include nasogastric (NG), gastrostomies (G-tube or button), nasojejunal (NJ), and gastro-jejunal (GJ) (also known as gastro-enteral) tubes. Tubes used less commonly, such as gastro-duodenal and orogastric tubes, are not discussed.
Other Names
Enteral feeding
Gastro-enteral tube
Gastro-jejunostomy
or GJ-tube
Gastrostomy or G-tube
Nasoduodenal or
ND-tube
Nasogastric or NG-tube
Nasojejunal or NJ-tube
Orogastric or OG-tube
Percutaneous endoscopic
gastrostomy or PEG
Billing & Coding
ICD-10-CM Diagnosis Codes
R63.3, Feeding difficulties (child >28 days)
Z93.1, Gastrostomy status
Z43.1, Encounter for attention to gastrostomy
Z46.59, Encounter for fitting and adjustment of other gastrointestinal appliance and device (e.g., replacement of nasogastric tube)
Z97.8, Presence of other specified device (e.g., nasogastric feeding tube)
Clinical Practice Guidelines
Adams RC, Elias ER.
Nonoral feeding for children and youth with developmental or acquired
disabilities.
Pediatrics. 2014;134(6):e1745-62. [Adams: 2014]
This clinical report provides (1) an overview of clinical
issues in children who have developmental or acquired disabilities that may
prompt a need to consider nonoral feedings, (2) a systematic way to support the
child and family in clinical decisions related to initiating nonoral feeding,
(3) information on surgical options that the family may need to consider in that
decision-making process, and (4) pediatric guidance for ongoing care after
initiation of nonoral feeding intervention, including care of the gastrostomy
tube and skin site; American Academy of Pediatrics.
Irving SY, Rempel G, Lyman B, Sevilla WMA, Northington L, Guenter P.
Pediatric Nasogastric Tube Placement and Verification: Best Practice
Recommendations From the NOVEL Project.
Nutr Clin Pract. 2018;33(6):921-927. [Irving: 2018]
This article provides consensus recommendations for best practices
related to nasogastric tube location verification in pediatric patients. These
consensus recommendations have been approved by the American Society for
Parental and Enteral Nutrition (ASPEN) Board of Directors.
Feeding Tubes
Differences among the various feeding tubes, gastrointestinal ostomies, and common concerns are addressed below. Decisions about placing and removing any tube that goes in the body can be difficult. It is important for families and medical personnel to discuss the benefits and possible risks associated with the various options before making a decision.
Oral Feeding vs. Tube Feeding
Feeding tubes are never considered “first-line” treatment. Indications for tubes are only considered after other routes of nutrition and/or hydration are not adequate to meet the child’s needs. Teaching young children to feed themselves and eating together as a family are deeply ingrained social norms. As such, families often prefer oral feeding over tube feeding, even if it takes a long time and requires additional preparation. Parents may not think of tube feeding as "eating." [Petersen: 2006] For various reasons, including the "unnaturalness" of tube feeding and other psychosocial concerns, parents may persist with oral feeding despite stressful or unenjoyable mealtimes and instructions from a physician to provide nothing by mouth. [Sullivan: 2000] [Petersen: 2006] Even in the absence of malnutrition, some patients have Pediatric Feeding Disorder (PFD) defined as impaired oral intake that is not age-appropriate and associated with medical, nutritional feeding skill, and/or psychosocial dysfunction [Goday: 2019]; children with PFD may require feeding tubes for supplemental nutrition. Children with feeding or enteral tubes typically need multidisciplinary providers and home health medical team as well as increased psychosocial support for the family. [Edwards: 2016]
Preliminary research suggests that a well-managed feeding tube usually (but not invariably) has a positive impact on nutritional status, but little is known about the overall impact of a feeding tube on a child’s or family's function long term. A systematic Cochrane review of gastrostomy tube feeding in children with CP does not support either tube or oral feeding over the long term; more study is needed. [Sleigh: 2004]
Indications for a Feeding Tube
Indications for a long-term or permanent feeding tube may include:
- Unsafe oral feeding. In some children, tube feeding may be necessary due to frequent coughing, choking, and aspiration. Even if maximum efforts are made to prevent aspiration of food and drink into the lungs (with gastrostomy tube feeding and less commonly, Nissen fundoplication), oral secretions may still be aspirated.
- A diagnosis of Pediatric Feeding Disorder and/or Avoidant/Restrictive Food Intake Disorder (ARFID), often characterized as “extreme picky eating."
- Recurrent periods of dehydration or weight loss due to frequent illnesses
- The need for an alternate route to give medications, fluids, persistent anorexia, or an unpalatable diet (ketogenic diet formulas). If malnutrition is present, oral feeds, even with nutritional supplementation, are rarely enough to resolve it. Sometimes, however, a period of tube feeding (nasogastric or gastrostomy tube) supplementation may allow the child to catch up to a normal weight and then continue with oral feeds alone.
- Percutaneous or surgical placement of a gastrostomy tube is recommended if the child will require long-term tube feeding. Despite their long-term use, these tubes are readily removable when no longer necessary.
- The child with a feeding tube can be fed by tube at night, supporting overall growth and hydration while allowing hunger and thirst to occur during the day so that oral feeding can continue. This may also be a time that oral-motor skills improve and oral feeds may be optimized, allowing a better transition back to oral feeding.
NG- and NJ -Tubes
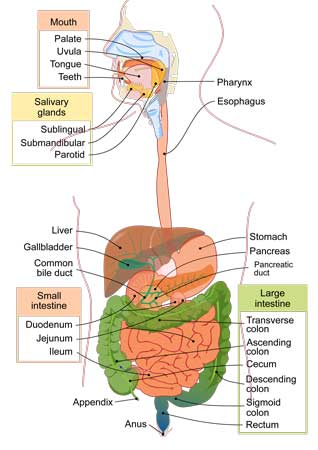
NG-tubes are placed by passing a thin, flexible tube through a nostril, down the back of the throat through the esophagus, and into the stomach (see diagram below). Once placed in the medical setting, parents or caregivers can be taught how to replace the tubes at home, and they often become more comfortable doing this than the child’s physician. The safest practice for determining the length of the NG-tube is to measure from the tip of the Nose, to the Ear, to the xyphoid process, and then to the Midline of the Umbilicus (the NEMU method) [Irving: 2018] and then marking this length on the tube that will be inserted.
The safest methods for NG-tube location verification include pH testing of gastric secretions (pH of 1–5.5 is indicative of correct placement) and radiography.
Liquid nutrition can be given through the NG feeds in larger intermittent amounts called boluses or over longer periods of continuous feeds (such as night feeds). Liquid nutrition can be delivered by gravity or with a pump, or pushed by syringe. Certain centers are exploring the benefits of NG-tubes to prepare infants to leave the neonatal intensive care setting and receive home tube feeding with close clinical follow-up. [White: 2020]
NJ tubes need to extend past the stomach into the small intestine. The first part of the small intestine is called the duodenum, and, ideally, the NJ tube extends past the duodenum to adequately deliver fluids beyond the stomach. For children who cannot have feedings into their stomachs, NJ tubes are often the next alternative. NJ feeds cannot be given as boluses; they require slower and longer feeding times (and are usually given by pump). One of the challenges to NJ tubes is that they can often curl up in the stomach unintentionally. NJ tubes are placed (and replaced) with the help of radiology, with an x-ray to confirm the placement is correct.
Both NG- and NJ-tubes can be easily dislodged or completely pulled out while a child is playing, moving around, or having care done. While the initial placement of a tube can make a child gag and feel uncomfortable, an NG or NJ tube is usually well-tolerated once the child becomes used to it. Other drawbacks include facial rashes from the adhesives on the face. Alternatives to facial adhesives include a bridle, which is a small piece of string that can anchor the tube behind the nasal bones and relieves the patient from irritating facial tape.
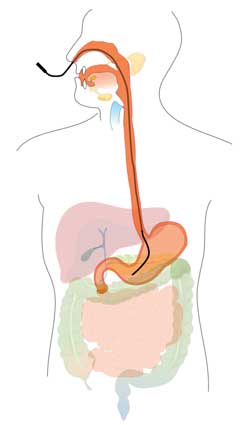
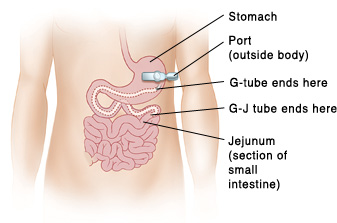
G-tubes & GJ-tubes
Ostomies generally refer to surgically created percutaneous pathways to enter or exit the body, such as a gastrostomy that is a pathway to the stomach, or a jejunostomy that is a pathway to the jejunum (part of the small intestine). A gastrostomy tube (G-tube) is a gastric feeding tube, passed through a gastrostomy, designed for liquid nutrients, fluids, or medication administration. Most of these procedures are now performed endoscopically or laparoscopically instead of as an open surgery.
G-tubes are placed in children who tolerate feedings into the stomach but cannot orally consume enough calories to maintain adequate nutrition and growth. These children are at risk for aspiration of oral feedings due to difficulty with oropharyngeal control, esophageal motility, and/or gastroesophageal reflux. [Sleigh: 2004] G-tubes can be changed when leaking or approximately every 6 months, though there is no expert consensus on how often to change a functioning G-tube.
There remains a lack of consensus on which infants should undergo G-tube placement. A recent study demonstrated no significant increase in hospitalizations or emergency room visits using an evidence-based oral-feeding protocol in infants and children <= 2 years old with oropharyngeal dysphagia and aspiration compared to those receiving feeds via G-tube. [McSweeney: 2020]
G-tube placement alternatives:
- Percutaneous endoscopic gastrostomy (PEG) - endoscope or image-guided radiography to ensure proper G-tube placement
- [Percutaneous] laparoscopically assisted gastrostomy (LAG or PLAG) (e.g., Seldinger technique)
- Stamm gastrostomy - open surgical procedure, higher rate of complications
- Janeway gastrostomy - conventional laparoscopic procedure, higher rate of complications
- Percutaneous radiological gastrostomy (PRG) – Interventional radiology-guided push-pull non-endoscopic placement directly through the abdominal wall
Many people use brand names to refer to their child’s device, but the generic terminology for the 2 styles is “balloon” and “non-balloon.” Common brand names include AMT MiniONE, MIC-KEY, and Bard. Ask for clarification if someone refers to a device that you are not familiar with.
Balloon-bolster low-profile gastrostomy device
- It contains an internal, water-filled balloon that holds the low-profile device in place and prohibits displacement.
- The balloon is breakable, so G-tube changes may be required more frequently than non-balloon devices.
- The valve is located on the outside of the body.
- It is relatively easy and painless to change.
- It has a feeding adapter locking mechanism.
Non-balloon button
- It contains a mushroomed-shaped tip which prevents displacement.
- The mushroom tip is less likely to break than the balloon tip, and therefore needs to be changed less frequently (once per year).
- The valve is located inside the stomach, making the non-balloon button less noticeable than the balloon device.
- It is more difficult to change and may require anesthesia to replace.
- It does not have a feeding adapter locking mechanism.
Feeding via a G-tube
- Care should be taken to select the appropriate formula. A consultation with local nutrition experts or pediatric gastroenterology may be helpful.
- Formula, approved blender diets, water, and liquid medications are the only fluids permissible through a G-tube. If a child uses thickeners to help reduce aspiration while drinking, the thickened fluids cannot be given through these tubes.
- The child should always be held upright during feeding.
- Oral stimulation (chewing, sucking on a pacifier) is recommended during the feed to promote a normal feeding environment and encourage regular stomach and intestinal motility.
- Participation at the dinner table and routine family eating activities should be performed during a G-tube feed to promote socialization.
- The G-tube should be flushed with water after each feeding to avoid obstruction due to drying of residual formula or medications. Recommended flushes are 5-10cc of water for infants and 15-30cc of water for older children.
- Most children who do not have a fundoplication repair should be able to burp and expel excess gas through their esophagus and mouth just like other children. If a child has neurologic delays or a fundoplication, venting can be done using an empty syringe, opening the extension catheter to drain air out, or with a specialized decompression tube for some buttons.
Medication Safety
Complications
Placement
- Major complications in a retrospective cohort of 208 patients with gastrostomy placement by interventional radiology included peritonitis (3%), [Dookhoo: 2016] and death (0.4%). [Friedman: 2004] Spearing or poking the transverse colon can occur, requiring surgery to fix.
- Minor complications in this cohort included tube dislodgement (37%), tube leakage (25%), and g-tube skin infection (25%). [Friedman: 2004]
- A review of 90 GJ-tubes placed at one center demonstrated complications
in <20% and included one intestinal perforation. Although there
were no procedural-related deaths, mortality was 23%, attributed in
part to the underlying medical fragility. [Onwubiko: 2017] Another study identified risk of perforation
at 9.4%, occurring most frequently in patients <10 kg, and
mortality risk at 0.9%/person. [Morse: 2017]
Pulling out the G-tube
- Children can pull-out their g-tube directly or inadvertently through contact or traction while playing.
- Dressing children in a "onesie" (a one-piece undershirt with the tube tucked inside) or placing the end of the tubing under the tabs of a disposable diaper can help avoid the tube being pulled out.
- Using an abdominal binder can also protect the tube from being pulled out.
- A dislodged GJ-tube typically requires fluoroscopy to replace.
Commercial vendors include many businesses started by entrepreneurial parents who recognized the need for adaptive and protective clothing to protect privacy and prevent tubes from being pulled out. The Medical Home Portal does not endorse any of these products but offers the following as an example of these resources.
- Adaptations by Adrian is a commercial site offering sales of adaptive clothing, including onesies, sizes small child to 2XL adult.
Leaking
- Leaking is a common problem with feeding ostomies. Ensuring that the tube is properly placed and, if there is a balloon, it is properly inflated can reduce leaking.
- Balloon style buttons for children vary in the volume contained in the balloon. Typically, this is 3 mL (cc) for infants up to 1 year and 5 mL (cc) for older children. If unsure, contact the physician who placed the button.
- Other factors that may affect the tube's fit include granulation tissue, damaged or displaced tubes, or outgrowing the tube size after weight gain. Leaking may also occur if the stomach expands or becomes full of fluids or air. When children are sick and/or their stomach does not empty easily, tubes may be more prone to leakage.
Ostomy Care
The site where the gastrointestinal tract (stomach or intestine) is pulled up to meet the skin heals into an opening called a stoma. There are many other kinds of ostomies not covered in this section, such as colostomies and ileostomies as exits for chyme (digested food and fluid) or stool, tracheostomies for respiration, and urostomies for removal of urine. Stoma nurses (or enterostomal teams) have specialized experience in caring for common problems, such as irritation or leaking.
Bathing
- Parents should clamp the g-tube or close the valve prior to bathing the child.
- Avoid overly hot water, which could irritate the surrounding skin.
- Use mild soaps and soft washcloths to avoid further irritation and abrasion.
Granulation tissue
- Granulation tissue represents a normal foreign body reaction in the skin surrounding the tube. It is red/pinkish, inflamed epithelial tissue that is firmer and more fibrous, like scar tissue.
- Seeing a wound clinic or ostomy nurse can be helpful for controlling and identifying causes of granulation tissue. Tubes should never be “tacked down” to one side of the abdomen for longer than a few hours, as this tension may worsen the granulation tissue or cause subcutaneous infections. • Excess granulation tissue can be controlled or reduced by topical application of triamcinolone cream 3 times daily for a week or cauterization using silver nitrate sticks obtained through a clinician.
Gastroesophageal reflux
- Overall there has been a trend away from concurrent anti-reflux surgery, such as fundoplication at the time of G-tube placement, as it is generally not indicated and presents safety and comorbidity risks.
- In one prospective observational study, 74% of children had reflux at the time of G-tube placement, and tube placement did not aggravate reflux in the majority of children. [Aumar: 2018] In this study, 11% of children developed GERD after G-tube placement, and 16% of the patients required anti-reflux surgery at a later time. [Aumar: 2018]
- Medical management is often sufficient to control reflux symptoms in tube-fed children rather than anti-reflux surgery.
- Transpyloric feeding via a jejunostomy or GJ-tube may decrease reflux symptoms but has its limitations, including slower, continuous feeding via pump and the need for imaging to replace the tube.
Role of the Medical Home
While most caregivers report “general satisfaction” with having had a feeding tube placed, many report the need to develop complex coping strategies over the first months to manage the equipment, feeding schedules, and care in addition to other parental responsibilities. The medical home provider is critical to helping with this process by:
- Facilitating family coping strategies
- Adjusting the child's diet for optimal growth and nutrition (and prevention of obesity)
- Adjusting the child's feeding schedule for optimal family/child functioning
- Monitoring the feeding tube for complications (feeding intolerance, reflux with aspiration, stoma leakage)
- Ensuring that the family has adequate equipment for using and caring for the feeding tube
- Ensuring that the family is aware of what to do if the tube dislodges
- Working with the family to ensure adequate and safe feeding during school, childcare, and respite care
- Helping the child and family continue to focus on advancing oral feeding by monitoring safety, prescribing oral motor therapy (if indicated), and optimizing the feeding schedule to enhance hunger during mealtimes
Resources
Information & Support
For Professionals
Enteral Nutrition Handbook, 2nd Edition (ASPEN)
Updated and expanded in 2019 to deliver the best of evidence-based recommendations, practical application, and hands-on clinical
skills along with the foundational science that underpins enteral nutrition. Available for a fee from American Society for
Parenteral and Enteral Nutrition.
Nutrition, 3rd Edition (Bright Futures)
Nutrition Issues and Concerns (Chapter 2) provides detailed guidance on breastfeeding and nutritional issues for children
with special health care needs. It includes a table with energy calculations for children and adolescents with Down syndrome,
spina bifida, Prader-Willi syndrome, cystic fibrosis, and pediatric HIV infection. Available for no cost as a downloadable
PDF or for a fee as a printed book.
For Parents and Patients
Feeding Tube Awareness Foundation
A very comprehensive, parent-focused site offering information about feeding tubes, their use, and troubleshooting. Downloadable
Tube Feeding parent guide in English and Spanish.
Nasogastric Tubes Insertion and Feeding (Nationwide Children’s Hospital)
Clear how-to info for families about NG-tube placement, feeding your child, and cleaning equipment.
Gastrostomy Tube Home Care (Cincinnati Children's Hospital)
Parent instructions on caring for a gastrostomy tube. Includes cleaning, flushing, giving meds, venting, protecting, and
problem-solving.
PEG Tube Home Care Instruction (Boston Children's Hospital)
Parent instructions on caring for a child after having a PEG or MIC-G tube placed.
Gastrostomy Feeding by Syringe (Cincinnati Children's Hospital)
Instructions and safety tips for gastrostomy feeding for parents. Also available in Spanish.
Gastrostomy-Jejunostomy Tubes (Cincinnati Children's Hospital)
Includes information about flushing, protecting, adding medications, and solving problems related to gastrostomy-jejunostomy
(G-J) tubes.
Patient Education
What You Need to Know Now: A Parent’s Introduction to Tube Feeding (Feeding Tube Awareness Foundation) ( )
)
A 26-page comprehensive guide for parents.
Tools
Insertion of a Mickey G-Tube Video
A 3½-minute video explaining how to insert a Mickey G-tube; Alberta Health Services.
NG Tube Insertion Video
A 7-minute video explaining how to insert an NG tube; Alberta Health Services.
Measuring a G-Tube Stoma Video
A 2½ min video explaining how to measure a stoma for replacing a G-tube; Alberta Health Services.
Services for Patients & Families Nationwide (NW)
| Service Categories | # of providers* in: | NW | Partner states (4) (show) | | NM | NV | RI | UT | |
|---|---|---|---|---|---|---|---|---|---|
| Dieticians and Nutritionists | 1 | 1 | 4 | 3 | 6 | ||||
| Pediatric Gastroenterology | 2 | 5 | 18 | 2 | |||||
| Pediatric Surgery [Discontinued] | |||||||||
For services not listed above, browse our Services categories or search our database.
* number of provider listings may vary by how states categorize services, whether providers are listed by organization or individual, how services are organized in the state, and other factors; Nationwide (NW) providers are generally limited to web-based services, provider locator services, and organizations that serve children from across the nation.
Helpful Articles
Braegger C, Decsi T, Dias JA, Hartman C, Kolacek S, Koletzko B, Koletzko S, Mihatsch W, Moreno L, Puntis J, Shamir R, Szajewska
H, Turck D, van Goudoever J.
Practical approach to paediatric enteral nutrition: a comment by the ESPGHAN committee on nutrition.
J Pediatr Gastroenterol Nutr.
2010;51(1):110-22.
PubMed abstract
Authors & Reviewers
| Author: | Jennifer Goldman, MD, MRP, FAAP |
| Reviewer: | Anna Ermarth, MD, MS |
| 2013: first version: Jennifer Goldman, MD, MRP, FAAPA |
Page Bibliography
Adams RC, Elias ER.
Nonoral feeding for children and youth with developmental or acquired disabilities.
Pediatrics.
2014;134(6):e1745-62.
PubMed abstract
Aumar M, Lalanne A, Guimber D, Coopman S, Turck D, Michaud L, Gottrand F.
Influence of Percutaneous Endoscopic Gastrostomy on Gastroesophageal Reflux Disease in Children.
J Pediatr.
2018;197:116-120.
PubMed abstract
Braegger C, Decsi T, Dias JA, Hartman C, Kolacek S, Koletzko B, Koletzko S, Mihatsch W, Moreno L, Puntis J, Shamir R, Szajewska
H, Turck D, van Goudoever J.
Practical approach to paediatric enteral nutrition: a comment by the ESPGHAN committee on nutrition.
J Pediatr Gastroenterol Nutr.
2010;51(1):110-22.
PubMed abstract
Dipasquale V, Catena MA, Cardile S, Romano C.
Standard Polymeric Formula Tube Feeding in Neurologically Impaired Children: A Five-Year Retrospective Study.
Nutrients.
2018;10(6).
PubMed abstract / Full Text
Dookhoo L, Mahant S, Parra DA, John PR, Amaral JG, Connolly BL.
Peritonitis following percutaneous gastrostomy tube insertions in children.
Pediatr Radiol.
2016;46(10):1444-50.
PubMed abstract
Edwards S, Davis AM, Bruce A, Mousa H, Lyman B, Cocjin J, Dean K, Ernst L, Almadhoun O, Hyman P.
Caring for Tube-Fed Children: A Review of Management, Tube Weaning, and Emotional Considerations.
JPEN J Parenter Enteral Nutr.
2016;40(5):616-22.
PubMed abstract
The purpose of this review is to summarize the multidisciplinary aspects of enteral feeding. The multidisciplinary team consists
of a variable combination of an occupational therapist, speech-language pathologist, gastroenterologist, psychologist, nurse,
pharmacist, and dietitian.
Friedman JN, Ahmed S, Connolly B, Chait P, Mahant S.
Complications associated with image-guided gastrostomy and gastrojejunostomy tubes in children.
Pediatrics.
2004;114(2):458-61.
PubMed abstract
Goday PS, Huh SY, Silverman A, Lukens CT, Dodrill P, Cohen SS, Delaney AL, Feuling MB, Noel RJ, Gisel E, Kenzer A, Kessler
DB, Kraus de Camargo O, Browne J, Phalen JA.
Pediatric Feeding Disorder: Consensus Definition and Conceptual Framework.
J Pediatr Gastroenterol Nutr.
2019;68(1):124-129.
PubMed abstract / Full Text
Using the framework of the World Health Organization International Classification of Functioning, Disability, and Health,
a unifying diagnostic term is proposed: "Pediatric Feeding Disorder" (PFD), defined as impaired oral intake that is not age-appropriate,
and is associated with medical, nutritional, feeding skill, and/or psychosocial dysfunction. By incorporating associated functional
limitations, the proposed diagnostic criteria for PFD should enable practitioners and researchers to better characterize the
needs of heterogeneous patient populations, facilitate inclusion of all relevant disciplines in treatment planning, and promote
the use of common, precise, terminology necessary to advance clinical practice, research, and health-care policy.
Heyman MB, Harmatz P, Acree M, Wilson L, Moskowitz JT, Ferrando S, Folkman S.
Economic and psychologic costs for maternal caregivers of gastrostomy-dependent children.
J Pediatr.
2004;145(4):511-6.
PubMed abstract
Irving SY, Rempel G, Lyman B, Sevilla WMA, Northington L, Guenter P.
Pediatric Nasogastric Tube Placement and Verification: Best Practice Recommendations From the NOVEL Project.
Nutr Clin Pract.
2018;33(6):921-927.
PubMed abstract
McSweeney ME, Meleedy-Rey P, Kerr J, Chan Yuen J, Fournier G, Norris K, Larson K, Rosen R.
A Quality Improvement Initiative to Reduce Gastrostomy Tube Placement in Aspirating Patients.
Pediatrics.
2020;145(2).
PubMed abstract / Full Text
Morse J, Baird R, Muchantef K, Levesque D, Morinville V, Puligandla PS.
Gastrojejunostomy tube complications - A single center experience and systematic review.
J Pediatr Surg.
2017;52(5):726-733.
PubMed abstract
Onwubiko C, Weil BR, Bairdain S, Hall AM, Perkins JM, Thangarajah H, McSweeney ME, Smithers CJ.
Primary laparoscopic gastrojejunostomy tubes as a feeding modality in the pediatric population.
J Pediatr Surg.
2017;52(9):1421-1425.
PubMed abstract
Petersen MC, Kedia S, Davis P, Newman L, Temple C.
Eating and feeding are not the same: caregivers' perceptions of gastrostomy feeding for children with cerebral palsy.
Dev Med Child Neurol.
2006;48(9):713-7.
PubMed abstract
Sandberg F, Viktorsdóttir MB, Salö M, Stenström P, Arnbjörnsson E.
Comparison of major complications in children after laparoscopy-assisted gastrostomy and percutaneous endoscopic gastrostomy
placement: a meta-analysis.
Pediatr Surg Int.
2018;34(12):1321-1327.
PubMed abstract / Full Text
Sleigh G, Brocklehurst P.
Gastrostomy feeding in cerebral palsy: a systematic review.
Arch Dis Child.
2004;89(6):534-9.
PubMed abstract / Full Text
Sullivan PB, Lambert B, Rose M, Ford-Adams M, Johnson A, Griffiths P.
Prevalence and severity of feeding and nutritional problems in children with neurological impairment: Oxford Feeding Study.
Dev Med Child Neurol.
2000;42(10):674-80.
PubMed abstract
White BR, Ermarth A, Thomas D, Arguinchona O, Presson AP, Ling CY.
Creation of a Standard Model for Tube Feeding at Neonatal Intensive Care Unit Discharge.
JPEN J Parenter Enteral Nutr.
2020;44(3):491-499.
PubMed abstract / Full Text