Acute Flaccid Myelitis (AFM)
- Prevalence
- Genetics
- Prognosis
- Practice Guidelines
- Roles of The Medical Home
- Clinical Assessment
- Diagnostic Criteria for Acute Flaccid Myelitis
- Differential Diagnosis
- Medical Conditions Causing Acute Flaccid Myelitis
- History & Examination
- Testing
- Treatment & Management of Acute Flaccid Myelitis
- Resources
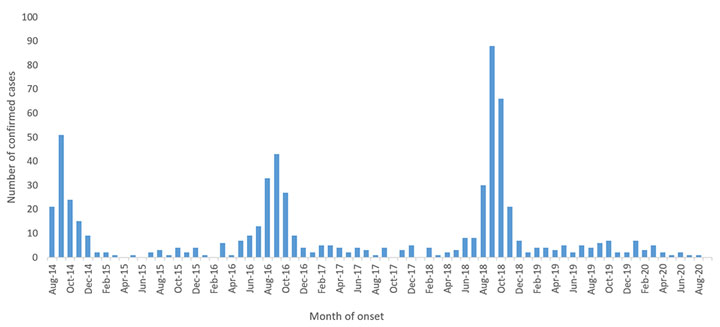
Acute flaccid myelitis is a rare but serious condition first identified in 2014. An increasing number of cases were reported of children presenting after a viral illness with focal flaccid paralysis and spinal cord abnormalities involving the gray matter. It has acted like an infectious process, similar to poliomyelitis caused by poliovirus, though it may rather be an inflammatory condition. Acute flaccid myelitis incidence has increased from August to November in even-numbered years. Since CDC surveillance began in 2014, the median age of affected children is 5.3 years with slightly more males than females. [Kidd: 2020] Upper extremities are affected more than lower extremities.
Prevalence
Because acute flaccid myelitis is a relatively new entity, its prevalence is not yet known. One retrospective study found an incidence of 2.4 cases per 100,000 hospitalizations/year prior to 2014. [Cortese: 2020] Since that time, acute flaccid myelitis incidence has increased from August to November in even-numbered years, suggesting viral epidemiology. Enteroviruses (coxsackie A16, EV-A71, and EV-D68) have been detected in the spinal fluid of a few patients, as have anti-enteroviral antibodies in some convalescent patients.
Genetics
Genetic susceptibility may play a role in acute flaccid myelitis occurrence, but this has yet to be identified. There are no known predisposing factors or genetic patterns noted to date.
Prognosis
Almost all children affected by acute flaccid myelitis will improve to some extent from the nadir of their weakness, but most do not return to their baseline level of functioning. Some children will remain severely disabled.
Practice Guidelines
CDC Clinical Guidelines were last updated in 2018 and are the only guidelines published. Basically, supportive care and neurological and infectious workup are recommended. No specific treatments are recommended, although some treatments are specifically not recommended.
Centers for Disease Control and Prevention.
Acute Flaccid Myelitis (AFM): Clinical Guidance for the Acute Medical Treatment of AFM.
National Center for Immunization and Respiratory Diseases, Division of Viral Diseases; (2020)
https://www.cdc.gov/acute-flaccid-myelitis/hcp/clinical-management.htm....
Roles of The Medical Home
The medical home should be alert to possible cases of acute flaccid myelitis but will more likely be managing the outpatient rehabilitation process after discharge from an inpatient unit than caring for the acute illness.
Clinical Assessment
The medical home should be alert to a child presenting in August through November with a history of a viral respiratory illness, usually with fever, and acute onset of weakness or new hand preference. Arms are affected more than legs, although about half present with gait difficulties. Neck, back, and affected extremity pain are common and cranial nerves are involved in about 20%; whereas, only 5% have altered mental status. Since respiratory failure can occur (about ¼ require ventilation), children should be referred immediately to an Emergency Department.
Presumptive and/or confirmed cases of acute flaccid myelitis should be reported to the CDC. For details of how to send information, see Acute Flaccid Myelitis - Data Collection (CDC).
After discharge, an initial neurologic exam is important to understand the child’s functioning, measure progress, and inform rehabilitation needs.
Diagnostic Criteria for Acute Flaccid Myelitis
Confirmed acute flaccid myelitis:
- Acute onset of flaccid paralysis of one or more extremity
- Gray matter predominant T2 hyperintensity of the spinal cord on MRI imaging
Probable acute flaccid myelitis:
- Acute onset of flaccid paralysis of one or more extremity
- Pleocytosis on lumbar puncture with or without confirmation of viral infection
Differential Diagnosis
Differential diagnosis includes transverse myelitis, acute disseminated encephalomyelitis (ADEM), and anything that affects the spinal cord acutely, such as infarction, compression, tumor, and other etiologies. Post-vaccination poliomyelitis is rarely encountered in children with immunodeficiency. Neurology consultation early on is recommended to differentiate among these conditions.
Transverse myelitis can easily be confused with acute flaccid myelitis. It is an immune-mediated inflammatory attack of the spinal cord and may represent the first episode of a chronic relapsing demyelinating condition. Weakness in this condition is typically bilateral, although it may be asymmetric. Although muscle tone may be diminished acutely, upper motor neuron problems, such as spasticity and hyperreflexia, are prominent [typically later on]. Sensory deficits are common. Transverse myelitis can also follow a viral illness.
ADEM is due to inflammation that affects both the brain and spinal cord, damaging the myelin that surrounds the nerve fibers.
Conditions that affect the spinal cord, such as compression by a tumor or a vascular lesion, will usually have a level below which the spinal cord is affected and the spinal cord above the level is normal. The compression may be asymmetric but usually involves sensory symptoms as well as pain. Acute spinal cord infarction can present with an anterior spinal cord syndrome in which flaccid weakness is a prominent feature. These conditions can be differentiated by spine MRI.
In practice, it is often very difficult to distinguish among AFM, acute myelitis, and acute spinal cord infarction, and clinical features and even imaging may show considerable overlap. The characteristic imaging features of AFM may be lacking on early imaging and the typical gray matter predilection only apparent on subsequent imaging studies (obtained several days or more after onset).
Medical Conditions Causing Acute Flaccid Myelitis
Non-polio enteroviruses, especially enterovirus D68 and A71, are thought to account for a large number of these cases and may account for the increase in frequency in even-numbered years. Additional viral causes include varicella, herpes simplex virus, West Nile virus, and cytomegalovirus.
History & Examination
If acute flaccid myelitis is suspected, evaluation by a pediatric neurologist should be sought emergently.
Current & Past Medical History
Developmental & Educational Progress
Social & Family Functioning
Physical Exam
Neurologic Exam
When there is initial suspicion of acute flaccid myelitis, look for quickly developing flaccid weakness and decreased or absent reflexes. Weakness may be found in all 4 extremities and is usually asymmetric. Arms are affected more often than legs, but only by a small margin. Proximal muscles are usually more affected than distal muscles. Sensory exam is intact in the majority of patients. Gait is usually abnormal. Many patients complain of pain in their affected extremities and/or back and neck pain. About 1/5 of patients have cranial nerve weakness. Most have normal mental status. [Centers: 2020]
After discharge from the hospital, categorize remaining difficulties in order to manage the rehabilitation process and calculate a baseline for monitoring progress. Watch the patient walk. Perform strength and sensory testing to characterize residual problems. Evaluations by Occupational and physical therapies may be helpful for moving forward.
Testing
Laboratory Testing
- Testing for viral etiologies
- Enterovirus
- Nasopharyngeal, oral and rectal swabs
- PCR in CSF and serum
- Other viruses
- Enterovirus
- Autoimmune etiologies
- Oligoclonal bands/CSF “MS Panel” in CSF and serum
- Anti-aquaporin 4 Abs in serum (“NMO testing”)
- Anti-MOG antibodies (serum)
Imaging
Other Testing
Subspecialist Collaborations & Other Resources
Pediatric Neurology
Emergent evaluation by a pediatric neurologist is warranted if acute flaccid
myelitis is suspected. See Pediatric Neurology
(see NW providers
[0]).
Pediatric Physical Medicine and Rehabilitation
Substantial residual weakness and difficulties in functioning should be managed by pediatric Pediatric Physical Medicine and Rehabilitation to help the child achieve optimal functioning. See Pediatric Physical Medicine & Rehabilitation (see NW providers [3]).
Treatment & Management of Acute Flaccid Myelitis
Centers for Disease Control and Prevention.
Acute Flaccid Myelitis (AFM): Clinical Guidance for the Acute Medical Treatment of AFM.
National Center for Immunization and Respiratory Diseases, Division of Viral Diseases; (2020)
https://www.cdc.gov/acute-flaccid-myelitis/hcp/clinical-management.htm....
For outpatient treatment, there is no specific treatment after the hospital admission; however, various therapies may be helpful, including physical therapy, occupational therapy, and, rarely, speech therapy. Attention to family functioning and the return to school are important.
Resources
Information & Support
For Professionals
Acute Flaccid Myelitis (CDC)
Information about Acute Flaccid Myelitis from the Centers for Disease Control and Prevention.
Patient Education
For Parents: Helping Children Who Have AFM (CDC)
Resources and information for parents of children with AFM from the Centers for Disease Control and Prevention.
Services for Patients & Families Nationwide (NW)
| Service Categories | # of providers* in: | NW | Partner states (4) (show) | | NM | NV | RI | UT | |
|---|---|---|---|---|---|---|---|---|---|
| Pediatric Neurology | 5 | 5 | 18 | 8 | |||||
| Pediatric Physical Medicine & Rehabilitation | 3 | 3 | 3 | 6 | 11 | ||||
For services not listed above, browse our Services categories or search our database.
* number of provider listings may vary by how states categorize services, whether providers are listed by organization or individual, how services are organized in the state, and other factors; Nationwide (NW) providers are generally limited to web-based services, provider locator services, and organizations that serve children from across the nation.
Helpful Articles
Messacar K, Schreiner TL, Van Haren K, Yang M, Glaser CA, Tyler KL, Dominguez SR.
Acute flaccid myelitis: A clinical review of US cases 2012-2015.
Ann Neurol.
2016;80(3):326-38.
PubMed abstract / Full Text
Morens DM, Folkers GK, Fauci AS.
Acute Flaccid Myelitis: Something Old and Something New.
mBio.
2019;10(2).
PubMed abstract / Full Text
Authors & Reviewers
| Author: | Lynne M. Kerr, MD, PhD |
| Reviewer: | Francis M. Filloux, MD |
| 2020: first version: Lynne M. Kerr, MD, PhDA |
Page Bibliography
Centers for Disease Control and Prevention.
Acute Flaccid Myelitis (AFM): Clinical Guidance for the Acute Medical Treatment of AFM.
National Center for Immunization and Respiratory Diseases, Division of Viral Diseases; (2020)
https://www.cdc.gov/acute-flaccid-myelitis/hcp/clinical-management.htm....
Centers for Disease Control and Prevention.
AFM: Initial Evaluation and Diagnostic Studies.
National Center for Immunization and Respiratory Diseases, Division of Viral Diseases; (2020)
https://www.cdc.gov/acute-flaccid-myelitis/hcp/clinicians-health-depar....
Centers for Disease Control and Prevention.
Case Definitions for AFM.
National Center for Immunization and Respiratory Diseases, Division of Viral Diseases; (2020)
https://www.cdc.gov/acute-flaccid-myelitis/hcp/case-definitions.html.
Cortese MM, Kambhampati AK, Schuster JE, Alhinai Z, Nelson GR, Guzman Perez-Carrillo GJ, Vossough A, Smit MA, McKinstry RC,
Zinkus T, Moore KR, Rogg JM, Candee MS, Sejvar JJ, Hopkins SE.
A ten-year retrospective evaluation of acute flaccid myelitis at 5 pediatric centers in the United States, 2005-2014.
PLoS One.
2020;15(2):e0228671.
PubMed abstract / Full Text
Kidd S, Lopez A, Nix WA, Anyalechi G, Itoh M, Yee E, Oberste MS, Routh J.
Vital Signs: Clinical Characteristics of Patients with Confirmed Acute Flaccid Myelitis, United States, 2018.
MMWR Morb Mortal Wkly Rep.
2020;69(31):1031-1038.
PubMed abstract / Full Text
Messacar K, Schreiner TL, Van Haren K, Yang M, Glaser CA, Tyler KL, Dominguez SR.
Acute flaccid myelitis: A clinical review of US cases 2012-2015.
Ann Neurol.
2016;80(3):326-38.
PubMed abstract / Full Text
Morens DM, Folkers GK, Fauci AS.
Acute Flaccid Myelitis: Something Old and Something New.
mBio.
2019;10(2).
PubMed abstract / Full Text